Last update: November 6, 2025
5 minute read
What Is ‘Leaky Gut Syndrome’? Separating Medical Fact from Wellness Myth
Confused about whether leaky gut is a real medical condition or just another wellness buzzword? Here’s what science actually says, plus practical tips to support your gut health.

By Derick Rodriguez, Associate Editor
Edited by Dr. Dimitar Marinov, MD, RDN, PhD

Have you ever scrolled through wellness blogs or TikTok videos and stumbled upon claims about “leaky gut syndrome” being the root cause of fatigue, acne, anxiety, or even autoimmune diseases? If so, you’re not alone.
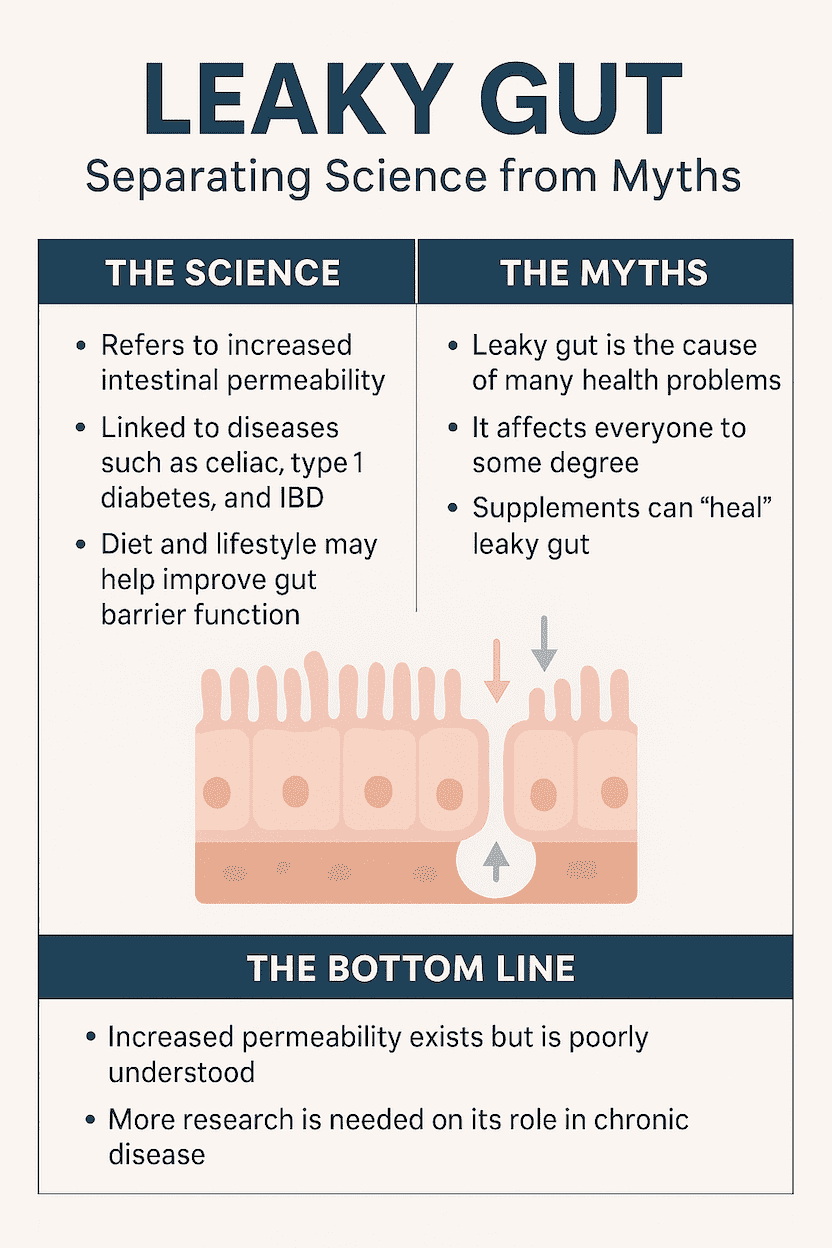
The term has exploded across the wellness world, but is it grounded in medical science, or is it mostly hype? Here’s the truth: while the concept of a “leaky” gut isn’t entirely made up, its role in chronic illness is far from settled.
In this article, we’ll break down what leaky gut actually is, what the research says, and how you can take evidence-based steps to support gut health without falling for pseudoscience.
Key takeaways
- “Leaky gut” refers to increased intestinal permeability, where the gut lining allows particles to pass into the bloodstream more easily
- It’s recognized in medical science, but only as a symptom, not as a standalone “syndrome”
- Research links increased gut permeability to conditions like IBD, celiac disease, and type 1 diabetes, but causation isn’t fully established
Understanding leaky gut
In medical terms, “leaky gut” refers to increased intestinal permeability, a state where the lining of your gut becomes less effective at keeping out harmful substances like toxins, bacteria, and undigested food particles.
Normally, the intestinal lining acts like a tightly woven net, allowing nutrients to pass through while keeping larger, unwanted molecules out. In leaky gut, tiny gaps open up, allowing foreign particles into the bloodstream and potentially triggering inflammation.
But here’s the catch: while scientists recognize increased gut permeability, the term “leaky gut syndrome” is not an official medical diagnosis.
Historical context: From fringe to front page
The concept of gut permeability isn’t new. In the 1980s, researchers discovered that people with celiac disease often had compromised gut barriers.
Since then, studies have explored links between permeability and conditions like Crohn’s disease, type 1 diabetes, and even autism spectrum disorders.
However, what’s changed in the past decade is marketing. Wellness influencers and supplement brands have positioned leaky gut as the hidden cause of everything from weight gain to brain fog, often oversimplifying complex science.
Conditions linked to increased gut permeability
Condition | Evidence Strength | Key Findings |
|---|---|---|
Celiac Disease | Strong | Gluten triggers intestinal barrier breakdown. |
Crohn’s Disease & IBD | Moderate | Higher permeability observed, but not always a cause. |
Type 1 Diabetes | Emerging | Studies suggest a possible early link in children. |
IBS (Irritable Bowel) | Mixed | Some patients show permeability changes; others don’t. |
Autoimmune Disorders | Hypothesized | More research needed before confirming causation. |
Bottom line: Increased permeability exists, but it’s usually a symptom, not the root cause.
How it works: The role of zonulin
One protein that’s been at the center of leaky gut research is zonulin, which is a human protein, identified as the precursor of haptoglobin-2, that can reversibly loosen the “tight junctions” between intestinal cells, increasing paracellular permeability.
- Zonulin is released in response to certain stimuli (e.g., bacterial components and gliadin fragments) and signals to the epithelial cytoskeleton to open junctions—part of normal, short-term barrier regulation.
- Elevated zonulin activity is best documented in celiac disease and is variably reported in type 1 diabetes risk cohorts; across IBS, obesity, and other conditions, findings are inconsistent and often conflicting.
- Most commercial “zonulin” ELISAs don’t specifically measure zonulin (pre-HP2); they pick up a mixture of zonulin-family peptides and can cross-react with other proteins such as properdin/complement C3. These assay results correlate poorly with functional permeability tests (e.g., the lactulose:mannitol ratio), so routine clinical use to diagnose “leaky gut” isn’t recommended.
— Dr. Dimitar Marinov, MD, RDN, PhD"Leaky gut syndrome" is not a recognized medical condition, despite its popularity in wellness circles. What science does acknowledge is increased intestinal permeability—a state where the gut barrier becomes less effective—which can occur as a symptom or consequence of certain diseases, such as celiac disease, inflammatory bowel disease, or type 1 diabetes. In these cases, permeability reflects underlying pathology rather than being the root cause itself.
Common wellness claims vs. medical evidence
Claim | Scientific Reality |
|---|---|
“Leaky gut causes acne, anxiety, and autoimmune disease.” | No strong evidence supports these claims. More research needed. |
“Everyone has some degree of leaky gut.” | Not necessarily. Most healthy people maintain a strong gut barrier. |
“You can heal leaky gut with expensive supplements.” | No supplement has been clinically proven to “seal” the gut lining. |
Best practices for supporting gut health
Even though “leaky gut syndrome” isn’t a diagnosis, improving gut barrier function supports overall wellness. Here’s what research suggests:
1. Focus on a whole-food diet
- Eat more fiber-rich foods like oats, legumes, vegetables.
- Include fermented foods like yogurt, kefir, and kimchi to support a healthy microbiome.
- Limit ultra-processed foods and added sugars, which may worsen gut inflammation.
2. Manage stress
Chronic stress affects the gut-brain axis and can increase permeability. Try:
- Mindfulness practices
- Breathwork or meditation
- Regular physical activity
3. Reduce alcohol intake
Excessive alcohol consumption is one of the most studied causes of increased gut permeability.
4. Be cautious with supplements
While probiotics and L-glutamine are often marketed as “gut-healing,” evidence remains mixed. Always discuss supplements with a healthcare provider first.
Get your personalized vitamin recommendations in less than 3 minutes.
Get your personalized vitamin recommendations in less than 3 minutes.
Safety & side effects
Be wary of self-diagnosing leaky gut and over-relying on supplements. Misdiagnosis can delay treatment for real conditions like celiac disease, IBD, or food allergies.
Seek professional care if you experience:
- Persistent bloating or abdominal pain
- Chronic diarrhea or constipation
- Unexplained fatigue or weight loss
Frequently asked questions (FAQ)
Here are some of the most frequently asked questions about leaky gut syndrome.
Final thoughts
Leaky gut may sound alarming, but context matters. While increased gut permeability is real, its role in chronic disease is still being studied, and quick-fix solutions rarely live up to the hype.
If you’re worried about your gut health, focus on proven habits: a balanced diet, stress management, and professional guidance when needed.
Empower yourself with evidence, not fear. The best path to gut health isn’t trendy, it’s sustainable.
Sources and references
- Leaky Gut Syndrome: Myths and Management - PMC
- Identification of human zonulin, a physiological modulator of tight junctions, as prehaptoglobin-2 - PubMed
- Widely Used Commercial ELISA Does Not Detect Precursor of Haptoglobin2, but Recognizes Properdin as a Potential Second Member of the Zonulin Family - PMC
Editor

Derick Rodriguez
Derick Rodriguez focuses on editing health and wellness-related content. With over half a decade of experience in the digital realm, Derick has developed a unique skill set that bridges the gap between complex health concepts and accessible, user-friendly communication. His approach is deeply rooted in leveraging personal experiences and insights to illuminate the nuances of health and wellness topics, making them more approachable and empowering readers with knowledge and confidence.
Fact checker

Dr. Dimitar Marinov
Dr. Marinov has years of experience in scientific research and preventive and clinical medicine. His publications in peer-reviewed journals are on nutritional status, physical activity, and musculoskeletal disorders among adolescents.
At VitaRx, we're not just passionate about our work — we take immense pride in it. Our dedicated team of writers diligently follows strict editorial standards, ensuring that every piece of content we publish is accurate, current, and highly valuable. We don't just strive for quality; we aim for excellence.
Related posts
While you're at it, here are some other relevant articles you might be interested in.

Get your personalized vitamin recommendations in less than
5 minutes.
Get your personalized vitamin recommendations in less than
5 minutes.






