Last update: November 6, 2025
10 minute read
Gut Health Probiotics: How to Strengthen Your Immune System with Research-Backed Supplements
Discover the role of gut health probiotics in improving immunity. Learn about research-backed strains and how to choose the best supplements for your needs.

By Derick Rodriguez, Associate Editor
Edited by Dr. Dimitar Marinov, MD, RDN, PhD

Unlock the secrets of a resilient immune system with a healthy gut. We often forget your gut houses trillions of microbes that play an important role in your body’s defenses.
Probiotics are live microorganisms you can add through foods or supplements for tangible health benefits. Explore our Probiotics Guide for more on how these helpful allies can change your gut health. Below, we’ll show you exactly how those microbes train your immune cells.
Key takeaways
- Probiotics are live microorganisms that offer health benefits when taken in enough amounts
- А well-balanced microbiome is crucial for training and changing immune responses
- Probiotics may support gut health by competing with unwanted microbes and helping maintain the epithelial barrier
Gut health & probiotics: Your path to improved immunity with Vitarx
If you want a stronger immune foundation, start in your gut; that’s where trillions of microbes interface with your body’s defenses, 24/7. Probiotics are live microorganisms that, when taken in enough amounts, can give a health benefit, and they’re found in foods like yogurt and carefully created supplements, backed by new evidence.
In plain English, this means: Commonly used daily doses range from about 1–20 billion CFU/day for healthy adults (strain- and product-dependent). In foods, look for “live and active cultures” on the label.
Nurture the gut, and the immune system often follows; quality probiotics act as a lever, not a silver bullet.
Understanding your gut health
Gut health 101: Why your microbiome matters for immunity
Your GI tract hosts a diverse ecosystem—hundreds of species with microbial cell numbers on the same order of magnitude as your own cells—and this microbial community helps train and change immune responses, shaping what’s friend versus foe.
Researchers call this complex community your “microbiome,” and it’s a hot topic because shifts in its balance can ripple through digestion, skin, mood, and whole-body immunity, in real life and in the data.

Here’s why that matters: A large proportion of immune cells are associated with the gut (often estimated around 70%, though exact figures vary), so microbial “training” influences whole-body defense and tolerance.
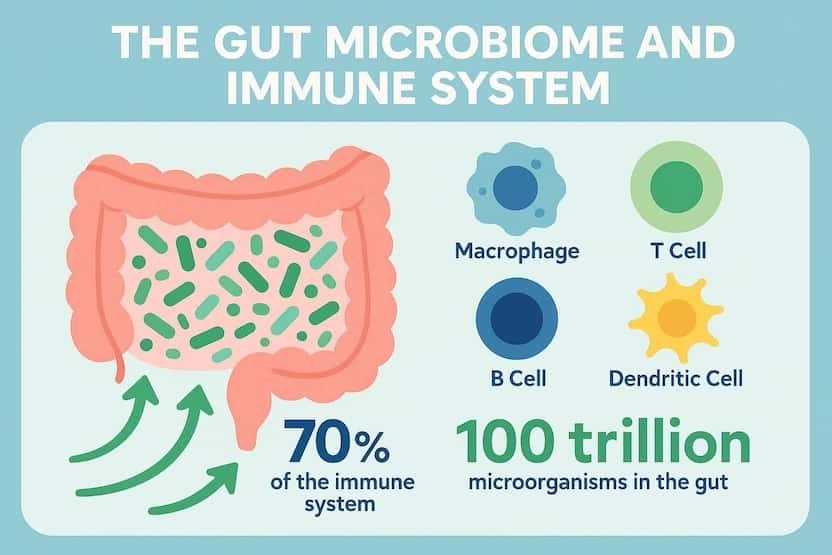
For background, a gastroenterology review describes how the enteric microbiota contributes to gastrointestinal health and notes the gut hosts hundreds of species with microbial cell numbers comparable to human cells.
But wait, what’s “microbiome” vs. “microbiota”? Microbiota = the microbes; microbiome = the microbes plus their genes and products (the full ecosystem blueprint).
A healthy microbiome is dynamic and diverse; think “well-tuned orchestra,” not “single instrument.”
How probiotics support your gut
Proposed mechanisms include:
- Competing with pathogens
- Helping strengthen the barrier
- Modulating immune responses, especially in the gut mucosa.
Some strains may contribute to short-chain fatty acid dynamics (directly or by supporting resident microbes), and certain strains can synthesize small amounts of vitamins, and many have shown benefits in digestion and regularity, depending on the context.
The bottom line: Mechanisms are strain-specific, and outcomes depend on dose, duration, and your baseline, so personalization matters.
Think of it this way: Short-chain fatty acids (like butyrate, acetate, propionate) fuel colon cells, tighten gut barriers, and help calm inflammation—one reason fiber-plus-probiotics is a good match.
Research highlights potential anti-inflammatory effects and roles in both innate and adaptive immunity, showing how specific probiotic strains can change host responses in targeted ways.
Here’s why that matters: Two products with the same “species” can work differently if the strain IDs differ; where evidence exists, match the exact strain to your goal.
Probiotics don’t replace your microbiome, they nudge it in a better direction when you pick the right tool for the job.
— Dr. Dimitar Marinov, MD, RDN, PhDYour gut microbiome is deeply connected to immune health, as a large proportion of immune cells are located in the gastrointestinal tract. Probiotics can support this system by strengthening the intestinal barrier, competing with harmful microbes, and fine-tuning immune responses. The benefits, however, are strain-specific—what works for one condition may not work for another.
Breaking down probiotic strains
Different genera and strains do different jobs, so picking a probiotic is like selecting the right athlete for the sport, not just the strongest athlete overall. Here’s a quick snapshot (keep in mind strain precision matters):
Strain/Genus (Example) | Potential Support Area | Notes |
|---|---|---|
Lactobacillus rhamnosus GG (LGG) | Skin and immune modulation | Evidence suggests it may help reduce risk or severity of atopic dermatitis in some contexts, especially early life, although results are mixed and effects are generally modest |
Bifidobacterium animalis subsp. Lactis (DN-173 010) | Regularity and GI comfort | Studied in fermented dairy; supports gut transit and comfort in some users, context matters |
Bifidobacterium longum 35624 | IBS-related comfort | Research suggests symptom support for IBS, strain-specific effect |
Saccharomyces boulardii | Antibiotic- and traveler’s diarrhea | Yeast probiotic with evidence for certain diarrheal contexts, dosing and timing matter |
Lactobacillus reuteri (specific strains) | Infant colic | Some strains show benefit in breastfed infants, niche use case |
So, how do you translate those names on a bottle?
Still scratching your head about names? Format is Genus species strain (e.g., Lactobacillus rhamnosus GG). That last tag (GG) is the evidence-carrying fingerprint.
Strain naming conventions and examples like LGG, DN-173 010, and 35624 are listed in NIH health professional resources.
Name tags matter; probiotic benefits live at the strain level, not just the species.
What makes VitaRx unique
We build formulas around research-backed strains, clean excipients, and viability from bottle to gut because what survives your shelf and stomach determines outcomes.
Our approach is minimalist but targeted: we pick strains with published data, design for stability (think moisture/heat protection), and stress clarity so you know exactly what you’re taking, no fluff. My rule as a formulator: every ingredient earns its spot or it’s out, full stop.
Prefer products that guarantee CFU through the end of shelf life rather than only at manufacture; what counts is what’s alive when you take it.
Fewer, better strains, delivered effectively, beat crowded labels with fuzzy dosing.
Get your personalized vitamin recommendations in less than 3 minutes.
Get your personalized vitamin recommendations in less than 3 minutes.
Evidence-based benefits and research
We see encouraging data for specific goals like reducing the risk of antibiotic-associated diarrhea, supporting IBS-related comfort, and even shortening the duration of acute diarrhea by about a day on average in some studies, especially with the right strains.
There’s also some evidence of small reductions in the incidence or duration of certain respiratory infections in some healthy populations, while bigger claims for “healthy people for everything” are still developing.
Safety is strong for most healthy adults, but rare events can happen, and special populations like premature infants need medical oversight.
But IBS isn’t IBD: Probiotics may ease IBS symptoms for some; inflammatory bowel disease is different and needs clinician-directed care.
Some studies have shown bouts of acute diarrhea can be about a day shorter and that probiotics might reduce IBS symptoms.
Quick safety note: Higher-risk groups include people with central lines, severe illness, or immune system weakness; always check with your clinician first.
Use probiotics for specific jobs with known strains; treat them like precision tools, not talismans.
More adults are using probiotics
Usage of probiotics by adults increased substantially between 2007 and 2012 in U.S. Surveys (e.g., NHIS), rising from roughly 1–2% to about 3–4% of adults.
Choosing the right probiotic supplement
Here’s how I audit a probiotic in 30 seconds, and yes, this is exactly how we build at VitaRx, every time:
- Strain specificity: look for named strains (e.g., LGG, 35624), not just species, because details drive outcomes.
- Effective CFUs at end of shelf life: viability matters more than big numbers on day one, stability is king.
- Evidence alignment: the strain should match your goal (e.g., AAD, IBS comfort), not a generic promise.
- Clean formulation: minimal additives, allergen transparency, and tested for contaminants, no surprises.
- Delivery & storage: packaging and capsules that protect from heat, moisture, and stomach acid, consistency wins.
Still curious about CFU? It stands for “colony-forming units”—a count of live microbes likely to grow; commonly used daily ranges are about 1–20 billion CFU, but more isn’t always better. Effective doses in research range both lower and higher, depending on the strain
Evidence always points out that benefits are strain-specific and context-dependent, stressing the value of precise picking and dosing.
Here’s why that matters: If a label lists only species or “proprietary blend,” you can’t check dose-per-strain or match to evidence.
Transparency lets you repeat results; opacity makes your experience a coin toss.
Health made easy: your go-to resource for essential vitamins and supplements
Adding probiotics into your daily routine
- Take with meals: Make it part of a regular meal (often breakfast), unless your product says otherwise, habit hooks help.
- Pair with fiber: Include prebiotic fibers (veggies, oats, legumes) to feed the good guys, food is the platform.
- Travel smart: Pack shelf-stable options and keep them dry and cool, protect viability.
- Time around antibiotics: If your clinician okays it, separate probiotics from antibiotic doses by a few hours, timing matters.
- Track outcomes: Monitor stool consistency, bloating, energy for 2–4 weeks, then adjust, data beats guesses.
VitaRx Tip
Start low and go slow; if you notice extra gas/bloating in week one, halve the dose or take every other day, then raise it later.
Taking the next step toward better gut health
Useful understanding for daily wellness
Start with the basics: Whole-food fiber, hydration, sleep, movement—then layer a targeted probiotic matched to your goal, for 30 days of consistent use.
I keep a note on my phone: Meals, timing, effects. It’s low-tech, high clarity.
Here’s a quick target: 25–38 g fiber/day (women/men) from beans, lentils, oats, berries, greens; even small increases can help if you’re starting low.
Stack fundamentals with smart supplementation; measure, adjust, repeat.
If you’re ready to make gut health probiotics part of your playbook, explore VitaRx’s research-aligned options and find the strain profile that fits your goal, without the clutter.
Frequently asked questions (FAQ)
Here are some of the most frequently asked questions about probiotics and gut health.
Final thoughts
Probiotics may offer modest benefits for gut health, which can in turn influence immune function. Focus on strain specificity, evidence-based benefits, and consistency for best results. What changes will you embrace for your gut health today?
Sources and references
- Probiotics - Health Professional Fact Sheet (NIH ODS)
- Probiotics: Usefulness and Safety (NCCIH)
- StatPearls: Probiotics (NCBI Bookshelf)
- Probiotics: mechanism of action, health benefits and their application in food industries (PMC)
- Probiotics - Consumer Fact Sheet (NIH ODS)
- A Gastroenterologist’s Guide to Probiotics (PMC)
- Advances in Nutrition Review: Probiotics for Healthy People (ScienceDirect)
- Probiotics for the Prevention and Treatment of Antibiotic-Associated Diarrhea: A Systematic Review and Meta-analysis | Nutrition | JAMA
- AGA Clinical Practice Guidelines on the Role of Probiotics in the Management of Gastrointestinal Disorders
- The effect of probiotics on functional constipation in adults: a systematic review and meta-analysis of randomized controlled trials - ScienceDirect
- The effect of probiotics on functional constipation in adults: a systematic review and meta-analysis of randomized controlled trials - ScienceDirect
- Probiotics for preventing acute upper respiratory tract infections - PubMed
Editor

Derick Rodriguez
Derick Rodriguez focuses on editing health and wellness-related content. With over half a decade of experience in the digital realm, Derick has developed a unique skill set that bridges the gap between complex health concepts and accessible, user-friendly communication. His approach is deeply rooted in leveraging personal experiences and insights to illuminate the nuances of health and wellness topics, making them more approachable and empowering readers with knowledge and confidence.
Fact checker

Dr. Dimitar Marinov
Dr. Marinov has years of experience in scientific research and preventive and clinical medicine. His publications in peer-reviewed journals are on nutritional status, physical activity, and musculoskeletal disorders among adolescents.
At VitaRx, we're not just passionate about our work — we take immense pride in it. Our dedicated team of writers diligently follows strict editorial standards, ensuring that every piece of content we publish is accurate, current, and highly valuable. We don't just strive for quality; we aim for excellence.
Related posts
While you're at it, here are some other relevant articles you might be interested in.

Get your personalized vitamin recommendations in less than
5 minutes.
Get your personalized vitamin recommendations in less than
5 minutes.









